
What is remote therapeutic monitoring?
In a further commitment to remote monitoring, CMS is now releasing and is asking for public comment on five codes that it describes as remote therapeutic monitoring (RTM). Although these codes have parallels to remote patient monitoring there are some important differences.
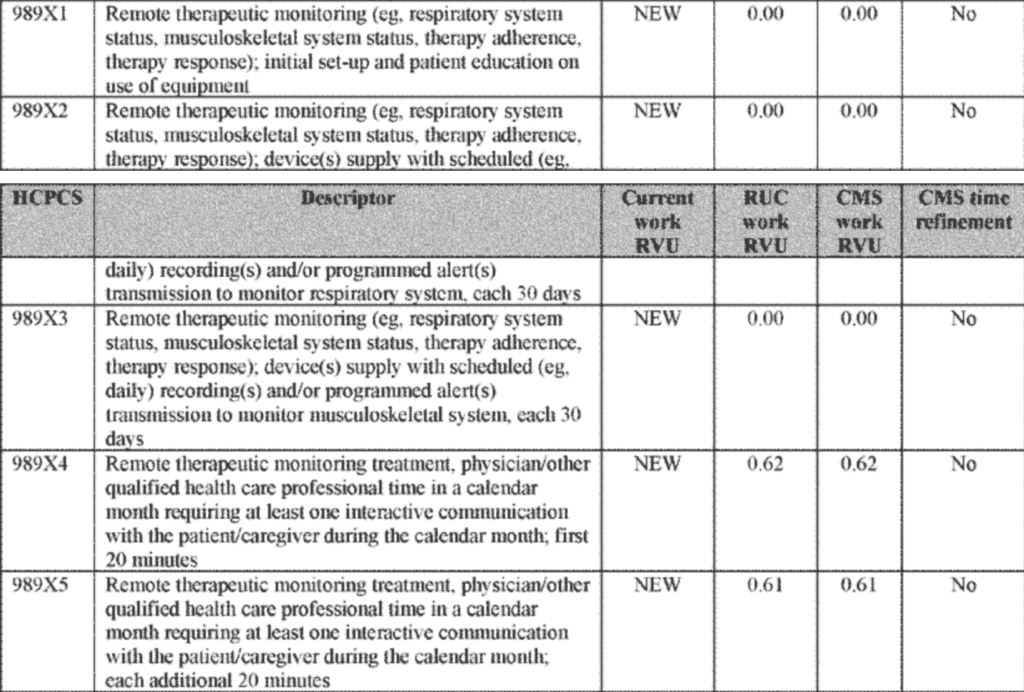
Table 1: RTM codes with their detailed explanation
An example of how RTM may be utilized in patient care would be to monitor patients with a pulmonary condition such as COPD and record how frequently the patient is compliant with the use of inhalers and other prescribed respiratory treatments. Environmental triggers could be correlated with apparent deterioration in a patient’s condition and subsequent therapeutic efficacy of treatments. Correlations between therapeutics used and treatment effect would also be key pieces of information.
To read the full excerpt from CMS in their proposed physician fee bulletin for 2022, please see below:
Source, CMS.gov:
Remote Therapeutic Monitoring (CPT Codes 989X1, 989X2, 989X3, 989X4, and 989X5)
Remote Therapeutic Monitoring (RTM) is a family of five codes created by the CPT Editorial Panel in October 2020 and valued by the RUC at its January 2021 meeting. The RTM family includes three PE-only codes and two codes that include professional work.
In recent years, we have finalized seven codes in the Remote Physiological Monitoring (RPM) family that include services similar to the new RTM codes. (See the CY 2021 PFS final rule at 85 FR 84542 through 84546 for more information.) Based upon our analysis, the services and code structure of RTM resemble those of RPM. For example, the RTM codes reflect similar staff and physician work, although the specific equipment used is different.
While there are notable similarities between the two sets of code descriptors, there are two primary differences. One difference is that according to RUC documents, primary billers of RTM codes are projected to be nurses and physical therapists. Stakeholders have suggested that the new RTM coding was created to allow practitioners who cannot bill RPM codes to furnish and bill for services that look similar to those of RPM. RPM services are considered to be E/M services and physical therapists, for example, are practitioners who cannot bill E/M services. The RTM codes, instead, are general medicine codes.
In our review of the new codes, we identified an issue that disallows physical therapists and other practitioners, who are not physicians or NPPs, to bill the RTM codes. By modeling the new RTM codes on the RPM codes, “incident to” services became part of the three direct practice expense-only (PE-only) codes (that is, CPT codes 989X1, 989X2, and 989X3) as well as the two professional work codes (that is, CPT codes 989X4 and 989X5). As a result, the RTM codes as constructed currently cannot be billed by, for example, physical therapists. We describe “incident to” services in the CMS Medicare Benefit Policy Manual, Chapter 15, beginning at section 60 and note that only physicians and certain other practitioners are authorized to furnish and bill “incident to” services. Incident to services are:
Additionally, we designated the treatment management RPM codes (that is, CPT codes 99457 and 99458) as care management services (84 FR 62697 through 62698), which allow general supervision rather than direct supervision for incident to services. The treatment management RTM codes (CPT codes 989X4 and 989X5), because they are not E/M codes, cannot be designated as care management services. As a result, we are seeking comment on how we might remedy the issues related to the RTM code construction in order to permit practitioners who are not physicians or NPPs to bill the RTM codes.
The second primary difference between the RTM and RPM codes is the nature of the data to be collected and how it is collected. According to the code descriptors, RTM codes monitor health conditions, including musculoskeletal system status, respiratory system status, therapy (medication) adherence, and therapy (medication) response, and as such, allow non-physiologic data to be collected. Reportedly, data also can be self-reported as well as digitally uploaded. RPM requires that data be physiologic and be digitally uploaded. We note that, for both sets of codes, the device used must meet the FDA definition of a medical device as described in section 201(h) of the Federal Food, Drug and Cosmetic Act (FFDCA). We are seeking comment on the typical type of device(s) and associated costs of the device(s) that might be used to collect the various kinds of data included in the code descriptors (for example, respiratory system status, musculoskeletal status, medication adherence, pain) for the RTM services.
For CY 2022, we are proposing the RUC-recommended work RVU of 0.62 for CPT code 989X4 (Remote therapeutic monitoring treatment management services, physician/other qualified health care professional time in a calendar month requiring at least one interactive communication with the patient/caregiver during the calendar month; first 20 minutes) and the RUC-recommended work RVU of 0.61 for its add-on code, CPT code 989X5 (Remote therapeutic monitoring treatment management services, physician/other qualified health care professional time in a calendar month requiring at least one interactive communication with the patient/caregiver during the calendar month; each additional 20 minutes (List separately in addition to code for primary procedure)) as a means of maintaining parity with the two RPM treatment management codes (CPT codes 99457 and 99458) upon which the two RTM codes are based. We also are proposing the RUC-recommended direct PE inputs for the two treatment management codes, CPT codes 989X4 and 989X5, without refinement.
We are proposing to refine the direct PE inputs for the three PE-only codes: CPT code 989X1 (Remote therapeutic monitoring (e.g., respiratory system status, musculoskeletal system status, therapy adherence, therapy response); initial set-up and patient education on use of equipment), CPT code 989X2 (Remote therapeutic monitoring (e.g., respiratory system status, musculoskeletal system status, therapy adherence, therapy response); device(s) supply with scheduled (e.g., daily) recording(s) and/or programmed alert(s) transmission to monitor respiratory system, each 30 days), and CPT code 989X3 (Remote therapeutic monitoring (e.g., respiratory system status, musculoskeletal system status, therapy adherence, therapy response); device(s) supply with scheduled (e.g., daily) recording(s) and/or programmed alert(s) transmission to monitor musculoskeletal system, each 30 days). We are proposing to value the PE for CPT code 989X1 by crosswalking to the PE RVU for RPM code 99453 upon which the new RTM code was based. We also are proposing to value the PE for CPT codes 989X2 and 989X3 by crosswalking to the PE RVU for comparable RPM code 99454, a code that includes payment for the medical device used to collect and transmit data. We note that the only input to CPT code 989X2 is a monthly fee of $25, which would not be paid as a direct cost under the PFS. Historically, we have considered most computer software and associated licensing fees to be indirect costs. However, as we noted in section II.B. of this proposed rule (the PE section), stakeholders have routinely expressed concerns with this policy, especially for evolving technologies that rely primarily on software and licensing fees with minimal costs in equipment or hardware.
Share This blog